Tacoma teacher grateful for outstanding cancer care
Laura Barber and her husband Jeff work at Annie Wright Schools in Tacoma. Jeff oversees the boarding program and Laura teaches 10th and 12th grade English.
“In her role as an educator, she is a pillar in our community, teaching young people how to write, analyze literature and be good citizens,” says Blair Irwin, MD, Laura’s medical oncologist.
As dedicated as Laura is to her students, she’s also dedicated to getting an annual mammogram. When she went for her yearly appointment in August 2019, she wasn’t expecting to have to go back for an ultrasound and biopsy.
“It was the day before the first day of school in 2019 when I got the results,” she says. “I felt 95 percent sure it wasn’t going to be cancer.”
Laura was 46 when she was diagnosed with breast cancer. She was devastated — and like many with this diagnosis, surprised by how it interrupted her life.
“No one plans for cancer,” Dr. Irwin says. “When this happens to a woman, it’s not part of their life plan. Something I do day in and out is to coach them through that interruption.”
Designing a treatment plan with listening and kindness
Laura met with MultiCare breast surgeon Bobby Stevens, MD, to discuss next steps. She was fearful she would need a mastectomy — something she wanted to avoid because of chronic upper back pain.
Then Laura found out the two areas of concern were close together in her right breast. In the end, she was able to choose between a lumpectomy and mastectomy.
“Dr. Stevens is amazing. He reassured me by answering all my questions and didn’t rush me at all during my appointments,” Laura says. “He wanted me to feel good about my decision and to know that it was my choice.”
A prior operation Laura had for Crohn’s disease had gone badly, making her terrified of surgery.
“I talked to Dr. Stevens’ nurse practitioner, Morgan Steele, ARNP, about my concerns and how scared I was. Just talking it through with her made me feel so much better,” she says. “She was such a good listener — so kind and helpful.”
Two days after surgery, Dr. Stevens called Laura with the results of the biopsy. It showed cancer in one lymph node, which meant she was not stage 1a, as they had previously thought, but stage 2b. It also meant she needed chemotherapy.
Personalized care, every step of the way
Laura missed the rest of the school year because of chemo. However, her school was understanding and supportive throughout her treatment.
“Annie Wright was amazing,” she says. “My students were so kind, visiting me and bringing me notes and gifts. Other teachers stepped up in my absence, and the principal and headmaster were incredibly supportive.”
Once a week for 24 weeks — before Christmas 2019 through May 2020 — Laura and her devoted husband Jeff made their way to the infusion suite at the MultiCare Cancer Institute for chemo.
“Although I know how lucky I am to have had such excellent care and that it was caught early, I felt angry for the first few months. It seemed like everyone at the cancer center had a walker or wheelchair,” she shares. “I thought, ‘Why am I here? Everyone else is in their 70s or 80s. Why am I the only 40-something in the room?’”
The cancer center offers counseling specifically for those undergoing cancer treatment. This helped Laura work through her anger.
“I saw Dr. Joseph Mitrovich. He is so knowledgeable about cancer, which helped me gain perspective,” she explains. “He had a huge impact on my life and my treatment.”
Laura also credits the infusion suite staff for helping her reframe her experience during chemo. Their kindness and willingness to go above and beyond had a positive impact.
“They couldn’t have been kinder,” she recalls. “They would remember me and the things we talked about. One of my nurses, Tammy Willison, was so reassuring and made me feel like I was getting special care. I nominated her for a DAISY award, and she won it.”
From the COVID-19 symptom screener to the front desk staff and the schedulers, Laura says it wasn’t just what they said — it was what they did.

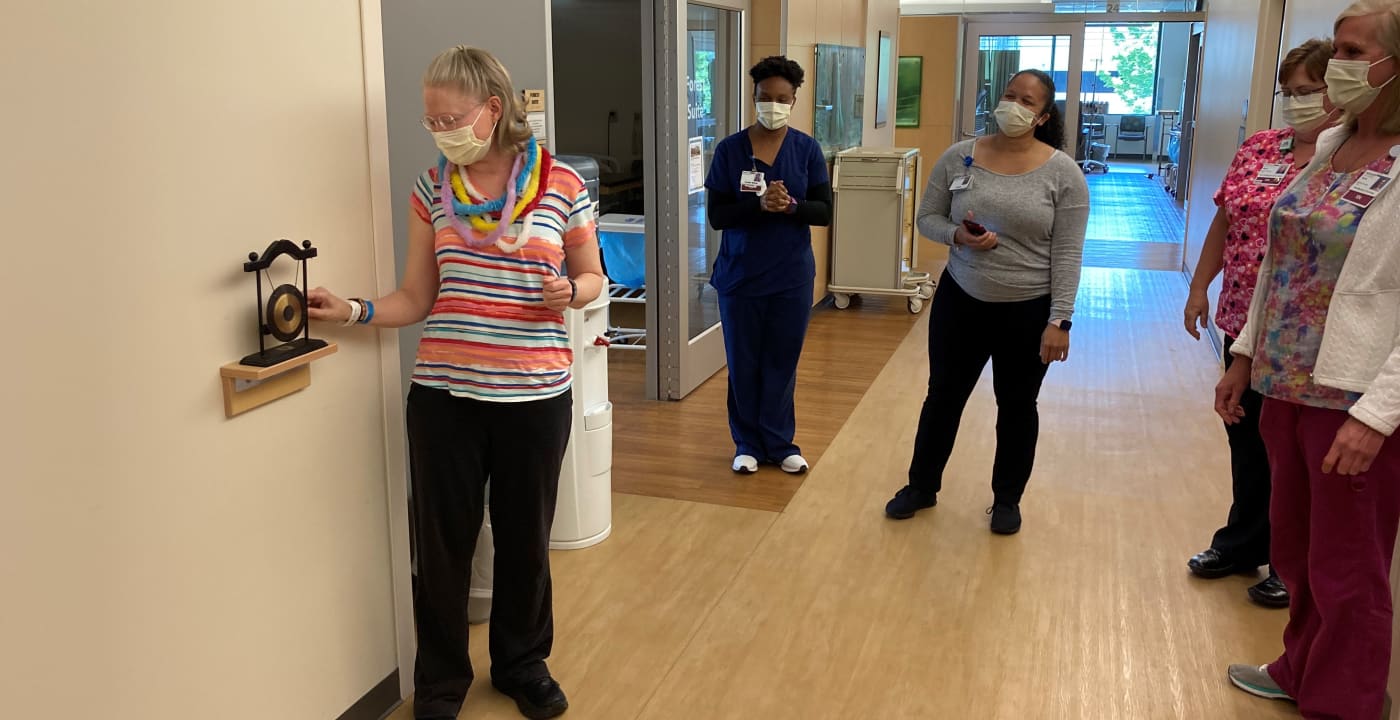
“They made me feel like they knew me, cared about me and wanted to see me,” she says. “I felt so appreciative of all the staff and wanted to do something for them. On my last day of chemo, I brought in a cake with everyone’s name on it.”
After chemo, Laura had radiation every weekday for five weeks.
“It was challenging to go in day after day. It’s really hard to go through, but, again, the kindness of the people and the professionalism made it as good as it could have been,” she says.
Maximizing quality of life during treatment
It was important for Laura to keep her quality of life reasonable to high during treatment so she could continue to exercise and have the energy to interact with others. But because the standard treatments for breast cancer can cause muscle aches and nerve pain, and Laura has underlying chronic disease and pain, Dr. Irwin worked diligently to find a regimen to mitigate and manage those side effects.
“That’s the art of oncology — maximizing quality of life in the face of diagnosis and the treatment that is required,” says Dr. Irwin.
However, Dr. Irwin explains it takes a multidisciplinary team to manage the myriad side effects of cancer treatment, including occupational therapists, lymphedema specialists, physical therapists, psychologists, social workers, financial counselors and more.
“I’m not an expert in all those areas. Our team has the ability to address these side effects, giving patients expertise in all domains of cancer care,” she adds.
Three years cancer-free
Because Laura’s cancer was found to be estrogen and progesterone positive, she’s required to be on hormone-blocking therapy for five years. She also receives a monthly shot to block estrogen, as she was unable to have both ovaries removed through surgery. Laura’s been getting these shots since June 2020.
“This means I have to go back to the infusion suite every month,” she explains. “Sometimes that is hard, since that’s where I received the chemo. The nurses are so awesome, though, and it’s nice to see them. I will have to continue with these shots until my bloodwork shows I’m fully in menopause.”
Laura is now three years cancer-free. Every July, she’ll have a mammogram and a breast MRI every six months. After five years, she’ll be advised how frequently she will need to be checked.
“It’s because of her vigilance in following the screening algorithm of annual mammograms starting at 40 that we were able to catch it early, keep her disease-free and monitor her the way she deserves,” says Dr. Irwin.



