Colorectal cancer survivor urges people not to delay colonoscopies
According to the American Cancer Society (ACS), colorectal cancer is the third most common cancer diagnosed in men and women, excluding skin cancers.
And because colorectal cancer has become increasingly common in younger adults, in 2018 the ACS lowered the recommended age to begin screening from 50 to 45.
While there isn’t a definitive reason people are getting colorectal cancers at younger ages, more than half of these cancers can be linked to lifestyle choices, including smoking, drinking excessive alcohol, having extra body weight, not being physically active, and eating a lot of red or processed meats and not enough whole grains, fruits and vegetables.
Risk factors that can’t be controlled include a family history of colorectal polyps; having Type 2 diabetes, inflammatory bowel disease or hereditary conditions (such as Lynch syndrome); race and ethnicity (African Americans and those of Ashkenazi Jewish descent have a higher risk).
“About half of my patients at any given time are under the age of 50, with some in their 30s and even 20s,” says MultiCare colorectal surgeon Laila Rashidi, MD, FACS, FASCRS.
One of her patients, Craig Laslie, was diagnosed with colorectal cancer in 2020 at age 45.
“Three years ago, I was experiencing bleeding where you shouldn’t be bleeding,” says Laslie, now 48. “I had noticed this for a little bit, and I attempted to self-diagnose. I thought I had a hemorrhoid.”
Laslie, who works in human resources, also thought the bleeding might have been caused by stress, as he had gone through a layoff because of the COVID-19 pandemic and was about to start a new job.
But the bleeding wasn’t going away. In May 2020, Laslie went to see his family doctor, who referred him for a colonoscopy with gastroenterologist Darien Heap, MD. Dr. Heap found a tumor in the lower part of his rectum.
Immediately following the procedure, Laslie was told he had colorectal cancer.
“Of course, I didn’t expect to hear that,” he says. “I’m a generally healthy person, and this is not something that runs in my family.”
Laslie was referred to oncologist Joseph Ye, MD. Once he underwent the required testing, he worked with Dr. Ye to devise a treatment plan, which included radiation, chemotherapy and surgery.
“There was a high level of concern about the size and location of the cancer, so I got started with treatment right away,” Laslie explains.
He had radiation treatment five days a week from June through August of that year, combined with daily oral chemotherapy.
“It was a challenging time, to say the least. Not only was this during the pandemic, but the treatment schedule was rigorous, and I had just started a new job,” says Laslie. “Thankfully, my new boss at the time was very flexible with me taking the time off for my treatments. I was fortunate to work with someone so understanding and supportive.”
When complex surgery requires the utmost expertise
Once radiation treatment was complete, Laslie was eligible for surgery. His sister — a nurse of 30 years — encouraged him to consider Dr. Rashidi for his surgery.
“My sister was a nurse at Madigan Army Medical Center at the time and knew of Dr. Rashidi’s expertise in the field of colorectal surgery, as she taught and performed robotic surgery procedures there,” explains Laslie. “And her good friend who’d had colorectal cancer surgery done by Dr. Rashidi had nothing but extremely positive things to say about her.”
He did some research of his own and determined it was a “no-brainer” to go with Dr. Rashidi. Surgery was scheduled for the end of October, but Laslie had to prepare during the month leading up to it.
“Dr. Rashidi and her team held my hand before, during and after surgery. Because it was a pretty major surgery, I had several pre-op appointments to help me prepare,” he says. “They were incredibly detailed as they walked me through the different steps of what to expect. There were certain preparatory tasks I had to do the week leading up to surgery and the night before.”
Because Laslie had a very low rectal cancer (the lowest part of the large intestine), it was close to the sphincter muscle, which controls bowel movements.
“Our goal, when oncologically possible, when the cancer is that low, is to preserve the sphincter so a person can have bowel movements on their own,” says Dr. Rashidi. “Not even five years ago, a case like Craig’s would have required a permanent bag [to remove waste]. But with the tools and the technology we have now, we can preserve the muscle and he can have a normal life without a bag.”
Laslie’s surgery — a robotic-assisted, ultra-low anterior resection, wherein the rectum is removed and the colon is attached to the anus — lasted four hours and is a type of surgery that requires exceptional precision.
With assistance from the da Vinci robot, Laslie’s procedure was less invasive, more precise, required fewer nights in the hospital and less pain medication in recovery than a traditional, open surgery.
After surgery, he had one more round of chemo from November 2020 through February 2021, which consisted of a daily oral pill and infusion once every three weeks.
Although Laslie did require a temporary ileostomy bag while healing, the bag was removed a few months after chemo was completed, and he says he was physically recovered by June 2021.
“Had the cancer been more progressed, things would probably be different for me from a quality-of-life standpoint,” adds Laslie. “If I had continued to wait, the cancer would have continued to grow, and I would have had fewer options from a surgical perspective.”
Disease-free and staying positive
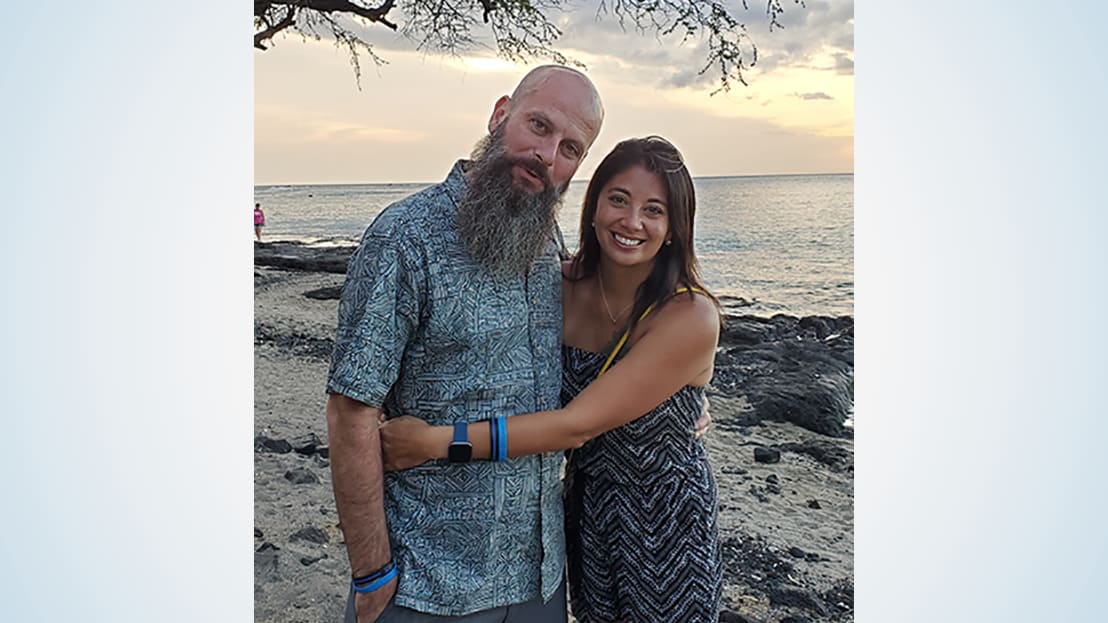
Throughout his cancer journey, Laslie, who lives with wife Tamra and two stepsons in Lacey, says, “Tamra is the reason I was able to get through this. She is my No. 1.”
“Craig and his wife were very positive and very engaged during his treatment,” says Dr. Rashidi. “He had a fantastic support system in her. She came with him to his appointments, took notes and asked questions. She was on top of things.”
And since completing treatment, Laslie says he’s had a very regimented surveillance plan.
“It has been so great to have all these follow-up appointments; everyone cares so much,” he says. “I continue to be disease-free and receive positive reports at all my checkups.”
In fact, at Laslie’s follow-up colonoscopy last year, Dr. Heap told him everything looked great and also shared a comment he wasn’t expecting.
“Dr. Heap said he could tell Dr. Rashidi had performed my surgery. He even brought in the other doctors in the practice to show them what an amazing job she had done,” he says. “That was pretty special. I knew I had made the right decision choosing her as my surgeon.”
Dr. Rashidi emphasizes the importance of getting screened and not ignoring symptoms.
“Colorectal cancer is treatable with great results, if you identify it soon enough,” she says. “When you’re young you don’t think of cancer, but it’s important to pay attention to symptoms and changes in your body.”
Laslie’s message echoes that of Dr. Rashidi: “Get screened, even if you have slightest of symptoms. And don’t self-diagnose like I did — talk to a medical professional.”




